Find The Best Thyroid Specialist Doctors in Dhaka, Bangladesh (BM&DC Verified)
Are you looking for a reliable thyroid specialist doctor in Dhaka? Bangladesh Health Alliance (BHA) c nonnects patients with BM&DC-verified thyroid experts who specialize in conditions such as hypothyroidism, hyperthyroidism, thyroid nodules, goiter, and thyroid cancer.
Why It Matters: Around the world, thyroid disorders affect an estimated 200 million people. In Bangladesh, research suggests that 15–20% of adults, especially women, experience thyroid-related health problems (Research Source). Early detection and proper treatment can prevent serious complications, including heart disease, infertility, and cancer.
Our listed doctors are highly experienced and affiliated with leading hospitals and clinics in Dhanmondi, Gulshan, Uttara, Malibagh, Mirpur, and across Dhaka.
Take the next step toward better health by booking your thyroid appointment online today. Book Thyroid Appointment Online
Top 10 Thyroid Surgeons in Dhaka – Thyroidologist Near You
Here is a selection of the most trusted and experienced thyroid doctors in Dhaka, verified by BHA:
Top 10 BM&DC-Verified Thyroid Specialists in Dhaka : Comparison Table
| Rank | Name of Specialist | BM&DC Reg. No. | Primary Specialization / Role | Key Credentials | BM&DC Status | Primary Affiliation | Years of Experience | Chamber Name | Visiting Hours | Appointment Number | Chamber Full Address (with Zip Code) | Google Map |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Prof. Dr. Indrajit Prasad | A-30944 | Professor & Head, Endocrinology (DMCH) | MBBS, FCPS, MD (Endocrinology), FACE (USA) | Verified | DMCH; Labaid Specialized Hosp. | 30+ Years | Labaid Specialized Hospital, Dhanmondi | 5pm–10pm (Fri off) | 10606 | House 06, Road 04, Room C-212, Dhanmondi, Dhaka 1205 | Google Map |
| 2 | Dr. M. Saifuddin | A-57289 | Associate Prof., Endocrinology (DMCH) | MBBS, BCS, MD (Endocrinology), 4×FRCP, FACE, FACP (USA) | Verified | DMCH; Labaid Specialized Hosp. | 20+ Years | Labaid Specialized Hospital, Dhanmondi | 5pm–9pm (Sat–Thu) | 10606 | House 06, Road 04, Dhanmondi, Dhaka 1205 | Google Map |
| 3 | Prof. Md. Faruque Pathan | A-6418 | Professor & Director, BIRDEM Academy | MBBS, MD (Endocrinology), FACE (USA) | Verified | BIRDEM General Hospital | 25+ Years | BIRDEM General Hospital, Shahbagh | 2:30pm–6pm (Sat–Wed) | 01847259771 | Room 210, Main Building, Shahbagh, Dhaka 1000 | Google Map |
| 4 | Prof. Dr. Md. Feroz Amin | A-24877 | Professor & Unit Head, Endocrinology (BIRDEM) | MBBS (DMC), MD (Endocrinology), FACE (USA) | Verified | BIRDEM; Labaid Specialized Hosp. | 22+ Years | Labaid Specialized Hospital, Dhanmondi | 6pm–9pm (Sat–Thu) | 10606 | House 06, Road 04, Dhanmondi, Dhaka 1205 | Google Map |
| 5 | Prof. Dr. Md. Ruhul Amin | A-21499 | Ex-Professor & Head, Endocrinology (DMC) | MBBS, BCS, MD (Endocrinology) | Verified | DMCH (ret.); Labaid Hosp. | 28+ Years | Labaid Specialized Hospital, Dhanmondi | 6pm–9pm (Sat–Thu) | 10606 | House 06, Road 04, Dhanmondi, Dhaka 1205 | Google Map |
| 6 | Dr. Syed Azmal Mahmood | A-66657 | Consultant Endocrinologist (DMCH) | MBBS, BCS, MD (Endocrinology), MACP, MACE (USA) | Verified | DMCH; Omnicare; JBF Hosp. | 15+ Years | JBF Hospital, Zigatola & Omnicare Mirpur | 3pm–5pm (Sat, Mon, Wed – JBF); 6:30–9pm (Sat–Wed – Omnicare) | 01713443360 / 01761901900 | JBF Hospital, Satmasjid Rd, Zigatola, Dhaka 1209; Omnicare, Begum Rokeya Sarani, Mirpur, Dhaka 1216 | Google Map |
| 7 | Dr. Faria Afsana | A-93614 | HOD & Assoc. Prof., Endocrinology (BIRDEM) | MBBS, DEM, MD (Endocrinology), FACE, MACP (USA) | Verified | BIRDEM General Hospital | 18+ Years | BIRDEM & Popular Diagnostic Center, Dhanmondi | 2:30pm–5:30pm (BIRDEM); 5:30–8:30pm (Popular) | 01407059574 / 09666787801 | Room 210, Main Building, Shahbagh, Dhaka 1000; Popular Diagnostic, House 16, Road 2, Dhanmondi, Dhaka 1205 | Google Map |
| 8 | Dr. Marufa Mustari | A-13233 | Asst. Prof., Endocrinology (BSMMU) | MBBS, FCPS (Endocrinology), MACE (USA) | Verified | BSMMU; Labaid; BRB Hosp. | 12+ Years | Labaid & BRB Hospital, Panthapath | 4pm–8pm (Labaid); 3pm–5pm (BRB) | 10606 / 01777764800 | Labaid House 06, Road 04, Dhanmondi, Dhaka 1205; BRB Hosp., 77/A East Rajabazar, Panthapath, Dhaka 1215 | Google Map |
| 9 | Asst. Prof. Dr. Nusrat Zarin | A-56825 | Asst. Prof., Endocrinology (BIHS) | MBBS, MD (Endocrinology) | Verified | BIHS; Ibn Sina Hosp. | 10+ Years | Ibn Sina Diagnostic & Consultation Center, Dhanmondi | 7:30–9pm (Sat–Wed) | 10615 | House 47, Road 10/A, Satmasjid Road, Dhanmondi, Dhaka 1209, 6th Floor | Google Map |
| 10 | Prof. Dr. Md. Sanowar Hossain | A-22234 | Sr. Consultant, Nuclear Medicine | MBBS, DNM (Nuclear Med), FRCP (Edin) | Verified | Labaid Specialized Hosp. | 30+ Years | Labaid Diagnostics, Dhanmondi | 2pm–8:30pm (Sat–Thu) | 10606 | House 01, Road 04, Dhanmondi, Dhaka 1205 | Google Map |
Specialist and Expertise
- Academic Leaders: Prof. Indrajit Prasad, Prof. Faruque Pathan, Prof. Feroz Amin, and Dr. Faria Afsana guide academic endocrinology at DMCH and BIRDEM, ensuring advanced thyroid care.
- Internationally Credentialed Specialists: Dr. M. Saifuddin and Dr. Syed Azmal Mahmood bring global training and fellowships, offering treatments aligned with international standards.
- Advanced Diagnostics: Prof. Md. Sanowar Hossain provides nuclear medicine expertise essential for thyroid cancer, nodules, and radioiodine therapy.
Key Centers of Excellence
- BIRDEM General Hospital (Shahbagh): National referral center for endocrinology; a WHO Collaborating Center.
- Dhaka Medical College Hospital (DMCH): Leading public hospital with a specialized endocrinology department.
- BSMMU: Premier postgraduate medical university offering advanced thyroid care.
- Labaid Specialized Hospital: Central hub for many senior professors’ private practices.
- Omnicare & Ibn Sina Hospitals: Accessible private centers with senior consultants.
Appointment & Contact Information
- Labaid Hotline: ☎️ 10606 (for Indrajit Prasad, Saifuddin, Feroz Amin, Ruhul Amin, Marufa Mustari, Sanowar Hossain).
- Popular Diagnostic Dhanmondi: ☎️ 09666787801 (for Indrajit Prasad, Faria Afsana).
- BIRDEM Chambers: ☎️ 01847259771 / 01407059574 (for Faruque Pathan, Faria Afsana).
- Omnicare Mirpur: ☎️ 01761901900 (for Syed Azmal Mahmood).
- JBF Hospital Dhanmondi: ☎️ 01713443360 (for Syed Azmal Mahmood).
- Ibn Sina Dhanmondi: ☎️ 10615 (for Nusrat Zarin).
Additional Notable Specialists
- Prof. Dr. Md. Farid Uddin – Professor & Chairman, Endocrinology (BSMMU).
- Prof. Dr. M.A. Hasanat – Senior Professor, Endocrinology (BSMMU).
- Prof. Dr. S.M. Ashrafuzzaman – Professor of Endocrinology, BIRDEM.
- Assoc. Prof. Dr. Shahjada Selim – Endocrinologist, BSMMU; consults in Uttara.
- Dr. Afroza Begum – Associate Professor of Endocrinology, DMCH.
Patient Advisory
- Always verify a doctor’s BM&DC registration number on the official portal before booking.
- For professors without public numbers, rely on institutional positions as proxy verification.
- Bring recent thyroid test results (e.g., TSH, T3, T4, ultrasound) to consultations for efficient care.
Did You Know? According to the Bangladesh Endocrine Society, thyroid disease is the second most common endocrine disorder in the country after diabetes. Women are up to eight times more likely than men to develop hypothyroidism.
Common Thyroid Disorders Treated in Dhaka
In Bangladesh, thyroid disorders are a major and often underestimated health crisis, affecting approximately 20–30% of the population. Over time, the problem has shifted from being mainly due to iodine deficiency to increasingly involving autoimmune conditions. Both rural and urban communities, including Dhaka, are affected, with women disproportionately impacted.
Overview of Thyroid Disorders in Bangladesh
- Hypothyroidism: The most prevalent disorder nationwide. Studies in Dhaka show prevalence rates of 7.0% for overt hypothyroidism and 3.8% for subclinical cases. Symptoms such as fatigue, weight gain, and depression are often dismissed as stress, especially in women. Untreated hypothyroidism can lead to infertility and pregnancy complications. Autoimmune thyroiditis, particularly Hashimoto’s disease, has replaced iodine deficiency as the primary cause. Congenital hypothyroidism also remains a critical concern.
- Hyperthyroidism: Less common (~1% prevalence). The leading cause in Dhaka is Graves’ disease. Symptoms include anxiety, weight loss, and palpitations, which are often subtle and lead to delayed or missed diagnosis.
- Iodine Deficiency and Goiter: The Universal Salt Iodization (USI) program significantly reduced goiter rates between the 1993 and 2004–2005 surveys. However, many lower-income and rural households still consume inadequately iodized salt.
Disparities in Care
- Access to Specialists: Facilities such as Dhaka Medical College Hospital and BSMMU provide specialist endocrine services, but rural populations face major challenges.
- Access to Diagnostics: Modern testing centers exist in Dhaka, but the costs remain high for many, particularly outside major cities.
- Barriers: Low public awareness, delayed diagnosis due to nonspecific symptoms, and stigma around women’s health issues hinder timely treatment.
Ongoing and Recommended Initiatives
- Screening Programs: Mandatory newborn screening for congenital hypothyroidism and routine pre-pregnancy screening for women are urgently needed.
- Health Education: Public campaigns should raise awareness about thyroid symptoms, promote iodized salt use, and emphasize the importance of early detection.
- Improving Access: Making diagnostic and treatment services more affordable and accessible, especially in rural areas, remains a pressing need.
Our thyroid specialists provide comprehensive diagnosis, treatment, and follow-up care for the full range of thyroid disorders. Each condition has distinct symptoms, risks, and treatment approaches:
Hypothyroidism (থাইরয়েড হরমোনের ঘাটতি)
- Global prevalence: Nearly 1 in 10 adults experience some form of hypothyroidism.
- Bangladesh context: Studies estimate 10–15% of Bangladeshi women aged 30–50 are affected, often undiagnosed until complications arise (Research).
- Symptoms: Fatigue, weight gain, dry skin, constipation, hair loss, irregular menstruation.
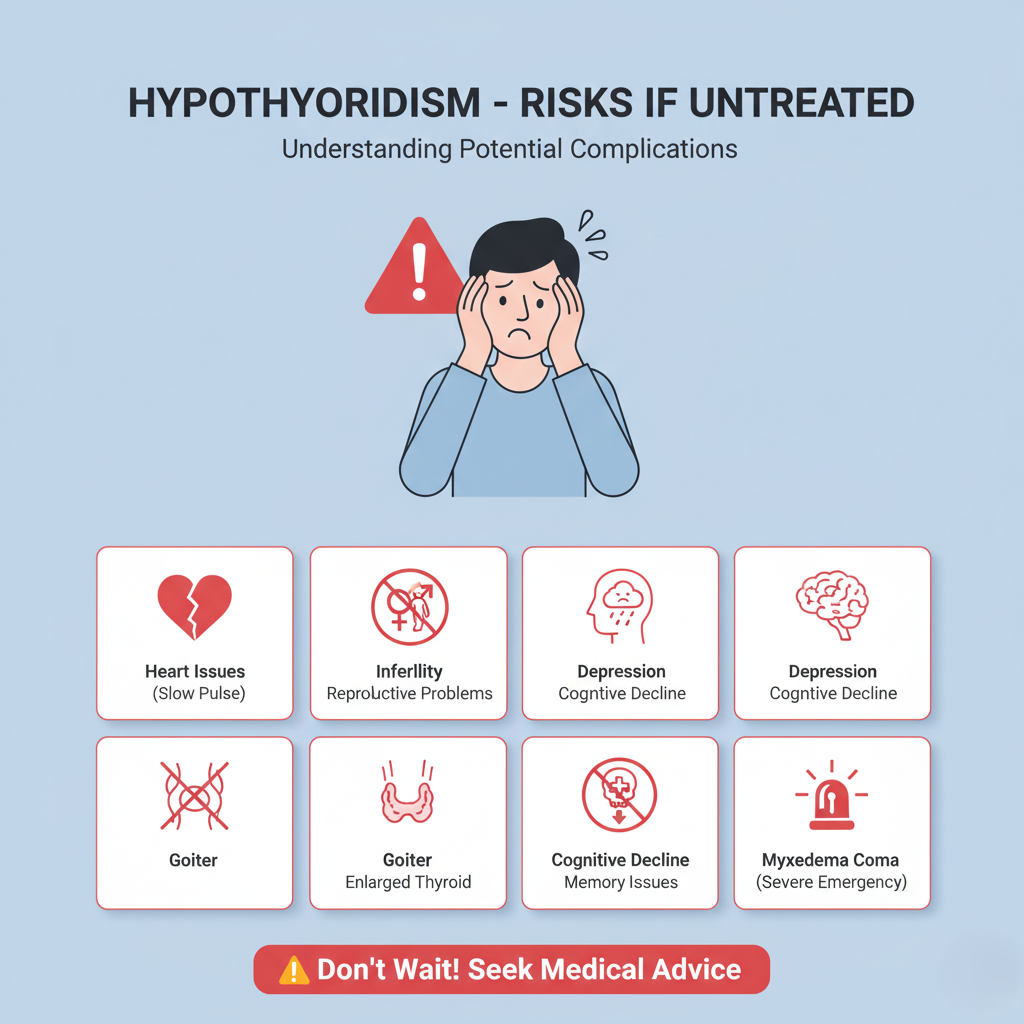
- Risks if untreated: Infertility, heart disease, depression, goiter, and in severe cases myxedema coma.
Treatment for Hypothyroidism:
Commonly caused by autoimmune Hashimoto’s thyroiditis or past thyroid treatments. The standard therapy is levothyroxine (Synthroid, Levoxyl, Levo-T), a synthetic T4 that mimics natural thyroid hormone. Dosage is adjusted by TSH levels and treatment is usually lifelong. It should be taken on an empty stomach 30–60 minutes before food. Some patients may be offered combination T4+T3 therapy or desiccated thyroid extract, though the latter is less commonly recommended.
Hyperthyroidism (থাইরয়েড হরমোন বেশি হওয়া)
- Global prevalence: Around 1–2% of the population worldwide (Research).
- Bangladesh context: More common in urban women aged 20–40; stress and iodine imbalance are contributing factors.
- Symptoms: Weight loss despite normal appetite, heat intolerance, palpitations, anxiety, bulging eyes (Graves’ disease).
- Complications: Arrhythmia, osteoporosis, and in rare cases thyroid storm, a medical emergency.
- Treatment for Hyperthyroidism: Antithyroid drugs (carbimazole, PTU), radioactive iodine, or surgery.
Thyroid Nodules & Goiter (গলার গিঁট / গয়টার)
- Prevalence: Bangladesh remains a high-risk iodine-deficient region; rural surveys show 10–12% goiter prevalence even after salt iodization programs.
- Nodules: Up to 50% of adults worldwide may develop nodules by age 60, though most are benign (Research).
- Risks: Cosmetic concerns, swallowing/breathing difficulties, risk of malignancy in 5–10% of nodules (Study).
- Diagnosis: Ultrasound, FNAC (Fine Needle Aspiration Cytology).
- Treatment: Monitoring, iodine supplementation, or surgery if nodules are large or suspicious.
Thyroid Cancer (ক্যান্সার চিকিৎসা)
- Global context: Accounts for 1–2% of all cancers, but is the most common endocrine malignancy (Research).
- Bangladesh trends: Hospital cancer registry data show rising thyroid cancer cases, especially among women aged 20–45.
- Types: Papillary, Follicular, Medullary, and Anaplastic.
- Survival rates: Papillary thyroid cancer has a 5-year survival rate above 95% when detected early (Research).
- Treatment for Thyroid Cancer: Surgery (thyroidectomy), radioactive iodine ablation, and lifelong thyroid hormone suppression.
Key Insight: In Bangladesh, thyroid diseases are often underdiagnosed due to limited routine screening. Awareness and regular check-ups can significantly improve outcomes.
Thyroid Care During Pregnancy & Fertility
Thyroid dysfunction during pregnancy is common and high-impact. Globally, 2–3% of pregnancies involve overt or subclinical thyroid disease. South Asian studies report 10–20% thyroid dysfunction among women of reproductive age (Research); Bangladesh data indicate a high burden of subclinical hypothyroidism and persistent iodine insufficiency in some areas, contributing to adverse outcomes.
Why Early Screening Matters
- Untreated thyroid disorders increase the risk of miscarriage (2–3× higher), preeclampsia, placental abruption, preterm birth, low birth weight, and impaired neurodevelopment in the child.
- Preconception or first-trimester detection and treatment greatly reduces these risks.
Who Should Be Screened
Women with any of the following should have a TSH test before conception or at the first prenatal visit:
- History of thyroid disease or surgery; goiter; thyroid antibodies
- Infertility or recurrent pregnancy loss
- Type 1 diabetes or other autoimmune diseases
- Prior preterm birth, preeclampsia, or postpartum thyroiditis
- Family history of thyroid disease
- Obesity, age >30, use of amiodarone/lithium, or iodine-deficient diet
(If universal screening isn’t feasible, risk-based screening is the strong minimum standard.)
Diagnostic Targets (Trimester-Specific)
- 1st trimester: 0.1–2.5 mIU/L
- 2nd trimester: 0.2–3.0 mIU/L
- 3rd trimester: 0.3–3.0 mIU/L
- Use local pregnancy-specific reference ranges where available.
Management at a Glance
Hypothyroidism (overt or subclinical with positive TPOAb):
- Treat with levothyroxine (LT4); safe in pregnancy & breastfeeding.
- If already on LT4, increase the dose by ~20–30% immediately after a positive pregnancy test (often +2 tablets/week), then titrate.
- Monitor TSH every 4 weeks until mid‑pregnancy, then once per trimester.
Hyperthyroidism (e.g., Graves’ disease):
- Use PTU in the 1st trimester, then switch to methimazole in the 2nd–3rd trimesters to reduce maternal hepatotoxicity.
- Aim for free T4 in the high-normal range. Avoid overtreatment.
- Beta‑blockers may provide short-term symptom relief.
Iodine & Nutrition:
- Pregnant and lactating women need ~250 µg of iodine per day. Use iodized salt. Consider prenatal vitamins with iodine where dietary intake is uncertain.
- Ensure adequate selenium, iron, and vitamin D.
Fertility & Preconception Planning
- Subclinical or overt hypothyroidism can cause anovulation and infertility. Treating to maintain TSH <2.5 mIU/L improves conception rates and reduces miscarriage risk.
- Women planning pregnancy after radioiodine therapy should wait 6–12 months and achieve stable thyroid function.
Postpartum Considerations
- Postpartum thyroiditis affects ~5–10% of mothers (higher if TPOAb+). Screen symptomatic mothers at 6–12 weeks postpartum or earlier if indicated.
- LT4 used during pregnancy is compatible with breastfeeding. Review dosage after delivery as requirements may decrease.
Red Flags — Seek Urgent Care
- Severe palpitations, chest pain, shortness of breath, or marked neck swelling
- High fever, agitation, or confusion (possible thyroid storm)
Bangla Micro‑Guide for Patient Handouts
- গর্ভাবস্থায় থাইরয়েড: প্রথম ১২ সপ্তাহে থাইরয়েড টেস্ট (TSH) করা ভাল।
- ওষুধ নিরাপদ: লেভোথাইরক্সিন গর্ভাবস্থায় ও বুকের দুধ খাওয়ানোর সময় নিরাপদ।
- ডোজ সমন্বয়: গর্ভাবস্থা শুরুতে ডোজ বাড়তে পারে; প্রতি ৪ সপ্তাহে টেস্ট করুন।
- আইোডিন: আইোডিনযুক্ত লবণ ব্যবহার করুন; প্রতিদিন পর্যাপ্ত পুষ্টি নিন।
Book Pregnancy-Safe Thyroid Consultation
Medical & Surgical Treatment Options for Thyroid
Treatment depends on diagnosis:
Treatment for Hypothyroidism (Underactive Thyroid)
Hypothyroidism is primarily caused by autoimmune Hashimoto’s thyroiditis or as a result of prior thyroid interventions. The standard first-line therapy is levothyroxine (Synthroid, Levoxyl, Levo-T). It binds thyroid receptors in cells, mimicking natural hormone and increasing metabolism. Dosage is titrated based on TSH and treatment is lifelong. It should be taken on an empty stomach 30–60 minutes before food. Some patients may benefit from combination T4+T3 therapy or desiccated thyroid extract, though the latter is less recommended due to inconsistency.
Treatment for Hyperthyroidism (Overactive Thyroid)
The goal is to suppress excess hormone production.
- Medications: Antithyroid drugs like methimazole and propylthiouracil (PTU) block hormone synthesis. Beta-blockers like propranolol control symptoms.
- Radioactive Iodine (RAI) Therapy: Involves swallowing radioactive iodine (I-131) which selectively damages thyroid cells (RAI info). Not used in pregnancy or breastfeeding.
- Surgery (Thyroidectomy): Removes part or all of the thyroid (thyroid surgery), recommended for large goiters, drug intolerance, or patient preference. Total thyroidectomy requires lifelong hormone replacement.
Treatment for Thyroid Cancer
Treatment strategy depends on cancer type and stage:
- Surgery: Total or near-total thyroidectomy; lymph node dissection if spread.
- Radioactive Iodine (RAI) Ablation: Destroys remaining thyroid tissue post-surgery.
- Thyroid Hormone Therapy: Replaces missing hormones and suppresses TSH to prevent cancer growth.
- External Beam Radiation: Used for advanced or RAI-resistant thyroid cancers.
- Chemotherapy & Targeted Therapy: Applied in advanced or anaplastic thyroid cancer. Targeted drugs block cancer growth pathways.
- Emerging Treatments: Transoral endoscopic thyroidectomy (scarless), novel antithyroid agents, immunomodulatory biologics, and liquid levothyroxine formulations (e.g., Tirosint-SOL) for better absorption.
Monitoring and Management
Effective thyroid treatment requires ongoing monitoring:
- Regular blood tests (TSH, T3, T4)
- Clinical symptom tracking (weight, energy, mood)
- Lifestyle support: adherence to medication timing, stress management, balanced diet, and adequate sleep.
Bangladesh Context: জাতীয় ক্যান্সার রেজিস্ট্রি ডেটা অনুযায়ী, ঢাকার প্রধান হাসপাতালগুলোতে মহিলাদের মধ্যে থাইরয়েড ক্যান্সার শীর্ষ ১০ ক্যান্সারের মধ্যে একটি। বাংলাদেশে প্রতি বছর আনুমানিক ৬,০০০–৮,০০০ নতুন থাইরয়েড ক্যান্সারের রোগী শনাক্ত হয় (সোর্স: NCBI)। বিশেষ করে ২০–৪৫ বছর বয়সী মহিলাদের মধ্যে এর হার দ্রুত বাড়ছে। গ্রামীণ এলাকায় সচেতনতার ঘাটতি ও নিয়মিত স্ক্রিনিং না থাকার কারণে অনেক রোগী দেরিতে শনাক্ত হন। শহরাঞ্চলে (ঢাকা, চট্টগ্রাম, রাজশাহী) তুলনামূলক বেশি শনাক্তকরণ হলেও, গ্রামে এখনো পর্যাপ্ত পরীক্ষার সুবিধা নেই।
Pediatric Thyroid Care in Dhaka
Why pediatric thyroid care matters
Children can develop thyroid disorders at birth or later in childhood. Globally, congenital hypothyroidism occurs in about 1 in 2,000–4,000 newborns (overview). In Bangladesh, limited routine newborn screening means many cases are detected late, increasing the risk of irreversible neurodevelopmental impairment.
Common pediatric thyroid conditions
- Congenital hypothyroidism: May be due to thyroid dysgenesis or dyshormonogenesis; early treatment within 2 weeks of life yields the best outcomes (reference).
- Autoimmune thyroiditis (Hashimoto’s): Increasingly recognized in school-age children and adolescents (info).
- Hyperthyroidism (often Graves’ disease): Presents with tachycardia, weight loss, irritability, sometimes eye signs (Graves’ disease).
Red flags in children
- Prolonged jaundice, large anterior fontanelle, constipation, poor feeding, hypotonia in newborns
- Poor growth, delayed milestones, learning difficulties, goiter in older children
Recommended tests and timing
- Newborn screening: Ideally 24–72 hours after birth (heel-prick dried blood spot for TSH ± T4) (screening basics).
- Confirmatory tests: Serum TSH, free T4, thyroid ultrasound/scintigraphy as indicated.
Treatment & follow-up
- Congenital hypothyroidism: Start levothyroxine 10–15 µg/kg/day immediately; aim to normalize free T4 within 2 weeks and TSH within 4 weeks; monitor every 2–4 weeks initially, then spacing out as age increases (guidance).
- Autoimmune hypothyroidism: Treat with weight-based levothyroxine; monitor growth, puberty, and learning.
- Pediatric hyperthyroidism: First-line antithyroid drugs (carbimazole/methimazole) with careful monitoring; beta-blockers for symptoms; definitive therapy (RAI/surgery) is individualized in adolescents (pediatric overview).
Dhaka care pathways & initiatives
- Where to go: Pediatric endocrine services are available at Dhaka Medical College Hospital, BSMMU (Pediatric Endocrinology), BIRDEM, and major private centers (Square Hospitals, Labaid).
- Local initiatives: Expansion of iodized salt coverage and hospital-based early screening pilots align with WHO/UNICEF recommendations on newborn screening and iodine nutrition (WHO iodine, UNICEF Bangladesh iodine).
Parent intents and problem-solving (what families need)
- Fast diagnosis: Clear guidance on where to test a newborn/child in Dhaka and expected timelines.
- Affordable care: Information on test packages, follow-up schedules, and generic LT4 availability.
- School support: Letters for teachers regarding medication timing, fatigue, and growth monitoring.
- Telehealth: Video follow-ups for dose adjustments to reduce travel burden.
Find Pediatric Thyroid Specialist
Emergency Thyroid Care (24/7)
When to seek emergency help
- Thyroid storm (life-threatening hyperthyroidism crisis): high fever, agitation, delirium, vomiting/diarrhea, severe tachycardia; untreated mortality 20–30% (clinical review).
- Myxedema coma: profound hypothyroidism with hypothermia, bradycardia, altered mental state (overview).
- Sudden neck swelling with breathing or swallowing difficulty, stridor, or voice change (possible hemorrhage, infection, or malignancy).
Immediate steps in Dhaka
- Call 999 (national emergency) and proceed to the nearest emergency department.
- Hospitals with 24/7 emergency & ICU: Dhaka Medical College Hospital, BIRDEM, Square Hospitals, Labaid, United Hospital.
What to bring
- Current medication list (antithyroid drugs, levothyroxine, beta-blockers)
- Recent lab reports (TSH, free T4/T3), ECG, imaging
- Contact details of your treating physician
Global best-practice stabilization
- Thyroid storm: Rapid beta-blockade, antithyroid drugs, iodine (after thionamide), steroids, fluid/electrolyte management, treat precipitating cause (ATA summary).
- Myxedema coma: ICU care, IV levothyroxine ± liothyronine, stress-dose steroids, active rewarming, manage triggers (review).
Patient intents & problem-solving
- Clarity: A one-click emergency call and clear map directions.
- Speed: Pre-arrival triage via hotline/tele-triage when available.
- Cost transparency: Estimated ER fees, potential ICU costs, and insurance/TPA desks at major hospitals.
Call Emergency Thyroid Helpline
Thyroid Screening & Preventive Health
Who should screen (Dhaka-focused)
- Women planning pregnancy or in the first trimester
- Individuals with family history of thyroid disease
- People with autoimmune disorders (e.g., type 1 diabetes)
- Newborns (ideally via heel-prick screening within 24–72 hours)
- Adults with symptoms: fatigue, weight change, palpitations, neck swelling
What to test and where
- Core tests: TSH, free T4, ± free T3, TPOAb/TgAb for autoimmune disease
- Imaging: Thyroid ultrasound for nodules/goiter; FNAC if indicated
- Where to test in Dhaka: Public tertiary centers DMCH, BMU, BIRDEM and accredited private labs (Square Diagnostics, Labaid Diagnostics)
Practical testing tips
- Morning sampling improves consistency; maintain same lab for follow-ups.
- Avoid biotin supplements for 48–72 hours before thyroid tests to prevent assay interference (advisory).
- Maintain consistent levothyroxine timing; do blood draw before daily dose when monitoring.
Prevention & population health
- Iodine nutrition: WHO notes iodine deficiency remains a leading preventable cause of thyroid disease globally, affecting ~2 billion people (WHO).
- Bangladesh initiatives: Universal Salt Iodization (USI), BSTI quality standards, and UNICEF partnerships continue to improve coverage (UNICEF Bangladesh).
Patient intents & solutions
- Convenience: Online appointment + home sample collection options.
- Affordability: Transparent package pricing and insurance acceptance where available.
- Continuity: Automated reminders for 6–12 month re-checks if at risk.
Consultation Fees & Packages
At-a-glance price ranges in Dhaka (public vs private):
- New patient consultation: Public hospitals BDT 200–500; private chambers BDT 800–1,800 (typical: BDT 1,000–1,200 in Gulshan/Baridhara; BDT 700–1,000 in Dhanmondi/Mirpur).
- Follow-up visit: Public BDT 150–300; private BDT 500–1,200.
- Tele-consultation: BDT 500–1,000 (video/phone) at many centers; some offer WhatsApp triage free.
- Ultrasound (thyroid/neck): BDT 1,200–2,800 (public lower, private higher).
- FNAC (needle test) of nodule: BDT 2,500–6,000 depending on imaging guidance.
- Core labs: TSH (BDT 400–800), free T4 (BDT 450–900), free T3 (BDT 450–900), TPOAb/TgAb (BDT 1,000–2,200 each).
- Radioactive iodine (RAI) ablation: BDT 35,000–90,000 depending on dose & facility (RAI overview).
- Thyroid surgery (thyroidectomy): Hemithyroidectomy BDT 65,000–120,000; total thyroidectomy BDT 100,000–200,000+ (surgeon fee, anesthesia, 1–2 nights stay; varies widely) (thyroid surgery).
Package examples (Dhaka diagnostics):
Many labs offer bundles starting BDT 1,200–2,500 (TSH+FT4±FT3). Add-ons: antibody tests, ultrasound, ECG if palpitations. Check accredited centers such as Square Diagnostics and Labaid Diagnostics.
Payment & access tips (Bangladesh-specific):
- Iodized salt/USI policy improves prevention (WHO iodine; UNICEF Bangladesh).
- Public hospitals follow DGHS policy; check DGHS OPD hours/fees.
- Private facilities accept bKash/Nagad/card; ask about package discounts and follow-up concessions.
Decision help — how to choose affordably:
- First diagnosis needed & budget tight → start at DMCH/BSMMU/BIRDEM OPD (low OPD fee; standard labs).
- FNA/RAI/surgery likely → choose tertiary hospital with nuclear medicine & endocrine-surgery teams.
- Pregnancy/pediatric cases → ensure facility has maternal–fetal or pediatric endocrine support.
- Tele-care acceptable → book video consult for dose titrations to reduce costs.
Thyroid Lifestyle & Diet Support
Daily targets (adults):
- Iodine: 150 µg/day; pregnancy/lactation 250 µg/day — use iodized salt; avoid excess (WHO iodine).
- Selenium: 55 µg/day — fish, eggs, nuts (NIH ODS selenium).
- Zinc: 8–11 mg/day — meat, legumes (NIH ODS zinc).
- Iron & vitamin D as needed after testing (NIH ODS iron; vitamin D).
Medication & food timing (to optimize levothyroxine):
- Take levothyroxine on an empty stomach with water; wait 30–60 min before food/coffee.
- Separate calcium/iron/soy/fiber supplements by ≥4 hours to avoid absorption issues.
- Biotin can distort lab tests; stop 48–72 h before bloodwork (biotin advisory).
Weight, sleep & activity goals:
- Aim for 5–10% weight reduction over 6 months if overweight (supports TSH control).
- Physical activity: 150–300 min/week moderate or 75–150 min/week vigorous + 2 days/week strength (WHO activity guideline).
- Sleep: 7–9 hours/night; consistent schedule improves metabolic health (CDC sleep).
- Stress reduction: Mindfulness, breathing, or yoga 10–20 min/day; consider referral for anxiety/depression management.
Goitrogens & practical diet notes:
- Cook cruciferous vegetables (cabbage, cauliflower, broccoli) to reduce goitrogenic compounds.
- Balanced intake of soy is acceptable if 4+ hours away from LT4 dose.
- Maintain adequate protein (1.0–1.2 g/kg/day) for muscle mass, especially with hypothyroid-related weight gain.
Patient intents & problem-solving (Dhaka context):
- Near-me diet support: Ask your hospital dietitian or reputable clinics (e.g., BIRDEM Nutrition) for individualized plans.
- Budget eating: Prefer iodized salt, small fish, lentils, seasonal vegetables; check BSTI-certified iodized salt brands (BSTI).
- Follow-up cues: If weight changes >2–3 kg in a month, resting HR >100 bpm, or neck swelling increases, book a review.
Bangladesh note: যদিও বাংলাদেশে সার্বজনীন লবণ আয়োডিনেশন (USI) কর্মসূচি চালু রয়েছে, তবুও অনেক গ্রামীণ অঞ্চলে এখনো পর্যাপ্ত আয়োডিনযুক্ত লবণ ব্যবহার করা হয় না। সাম্প্রতিক সমীক্ষায় দেখা গেছে যে নিম্ন-আয়ের পরিবারগুলির মধ্যে এখনো প্রায় ২০–২৫% ক্ষেত্রে আয়োডিনের ঘাটতি রয়েছে (UNICEF Bangladesh). তাই এই ঘাটতি দূর করতে USI নীতিমালার কঠোর বাস্তবায়ন এবং সচেতনতা বৃদ্ধির জন্য জনসাধারণের শিক্ষা কার্যক্রম অত্যন্ত গুরুত্বপূর্ণ। শহরাঞ্চলে তুলনামূলকভাবে পরিস্থিতি ভালো হলেও, গ্রামীণ ও প্রত্যন্ত এলাকায় লবণের গুণগত মান ও সরবরাহ নিশ্চিত করা একটি বড় চ্যালেঞ্জ হিসেবে রয়ে গেছে।
Get Diet Guidance for Thyroid Health
Frequently Asked Questions
Who is the best thyroid specialist doctor in Dhaka?
The best thyroid specialists in Dhaka are featured on Bangladesh Health Alliance (BHA). The platform highlights the top 10 BM&DC-verified thyroid doctors, including their degrees, hospital affiliations, experience, consultation fees, and patient ratings. This helps patients select the most trusted doctors for conditions such as hypothyroidism, hyperthyroidism, thyroid nodules, goiter, and thyroid cancer.
Can thyroid problems affect pregnancy?
Yes. Thyroid disorders during pregnancy can harm both mother and baby by increasing risks of:
- Miscarriage
- Preeclampsia
- Preterm birth
- Low birth weight
Specialized pregnancy-safe thyroid care in Dhaka is available at BSMMU, BIRDEM, and Square Hospital. Experts recommend TSH screening before conception and in early pregnancy for safer outcomes.
Is there a pediatric thyroid specialist in Dhaka?
Yes. Pediatric endocrinologists in Dhaka treat children with thyroid disorders such as congenital hypothyroidism, Hashimoto’s thyroiditis, and Graves’ disease. Key hospitals include Dhaka Medical College Hospital, BSMMU, and BIRDEM. Early diagnosis and treatment are vital to prevent long-term growth and developmental problems.
How much does it cost to see a thyroid doctor in Dhaka?
Typical costs include:
- Consultation fee: BDT 500–1,200
- Thyroid test packages: BDT 1,200–2,500 (TSH, T3, T4)
- Advanced imaging/FNAC: BDT 2,500–6,000
Affordable thyroid packages are available at Square Diagnostics and Labaid Diagnostics.
Can I book a thyroid doctor online in Bangladesh?
Yes. Patients can easily book online appointments through Bangladesh Health Alliance (BHA). The service offers both in-person visits and teleconsultations with verified thyroid doctors in Dhaka.
What are the symptoms of thyroid disorders?
Thyroid disorders can look different depending on age, gender, and life stage. Below is a user-friendly breakdown to help you identify key warning signs.
General Symptoms (All Patients):
- Fatigue and weakness
- Sudden weight gain or loss
- Irregular heartbeat or palpitations
- Hair loss, dry skin, brittle nails
- Infertility or irregular periods
- Neck swelling or goiter
Women:
- Menstrual irregularities
- Infertility and recurrent miscarriages
- Depression, mood swings, weight gain
- Hair loss and dry skin
Men:
- Fatigue and muscle weakness
- Weight fluctuations
- Decreased libido
- Hair thinning
Children:
- Delayed growth and puberty
- Learning and developmental delays
- Goiter or neck swelling
Pregnancy:
- Fatigue and palpitations
- Higher risk of miscarriage and preeclampsia
- Preterm birth if untreated
By Age Group:
- Children: Congenital hypothyroidism, learning and growth delays
- Young Adults (20–40): Autoimmune thyroiditis, infertility, weight issues
- Middle Age (40–60): Hypothyroidism, hyperthyroidism, often with diabetes
- Elderly (60+): Subclinical hypothyroidism, increased cardiovascular risks
By Region in Bangladesh:
- Urban (Dhaka, Chattogram): More diagnoses due to access to care
- Rural: Lower awareness, delayed diagnosis, iodine deficiency persists
- Coastal: Higher iodine intake from seafood, fewer goiter cases
- Northern districts: Historically high goiter rates, improving with iodized salt
If you notice these symptoms, see a thyroid doctor in Dhaka for timely testing and treatment.
How common are thyroid disorders in Bangladesh?
- 15–20% of adults in Bangladesh suffer from thyroid disorders.
- Women are 8 times more likely than men to be affected.
- A Dhaka study found 7% overt hypothyroidism and 3.8% subclinical hypothyroidism.
This confirms thyroid disease as a significant public health concern in Bangladesh.
Can thyroid disease be cured permanently?
- Hypothyroidism: Requires lifelong levothyroxine treatment.
- Hyperthyroidism: May be cured with medicines, radioactive iodine, or surgery.
- Thyroid cancer: Managed through surgery, radioactive iodine, and hormone therapy.
Some thyroid disorders can be permanently cured, but most hypothyroidism patients need ongoing treatment.
What foods are good for thyroid health?
- Iodine: Iodized salt, fish, and seaweed
- Selenium: Nuts, eggs, and fish
- Zinc: Meat, legumes, and grains
A qualified nutritionist in Dhaka can design a personalized thyroid-friendly diet.
When should I get a thyroid test in Dhaka?
Testing is recommended if you experience:
- Fatigue, weight changes, or hair loss
- Neck swelling or goiter
- A family history of thyroid disorders
- Pregnancy or plans for pregnancy
Trusted diagnostic labs include Square Diagnostics, Labaid Diagnostics, BIRDEM, and BMU.