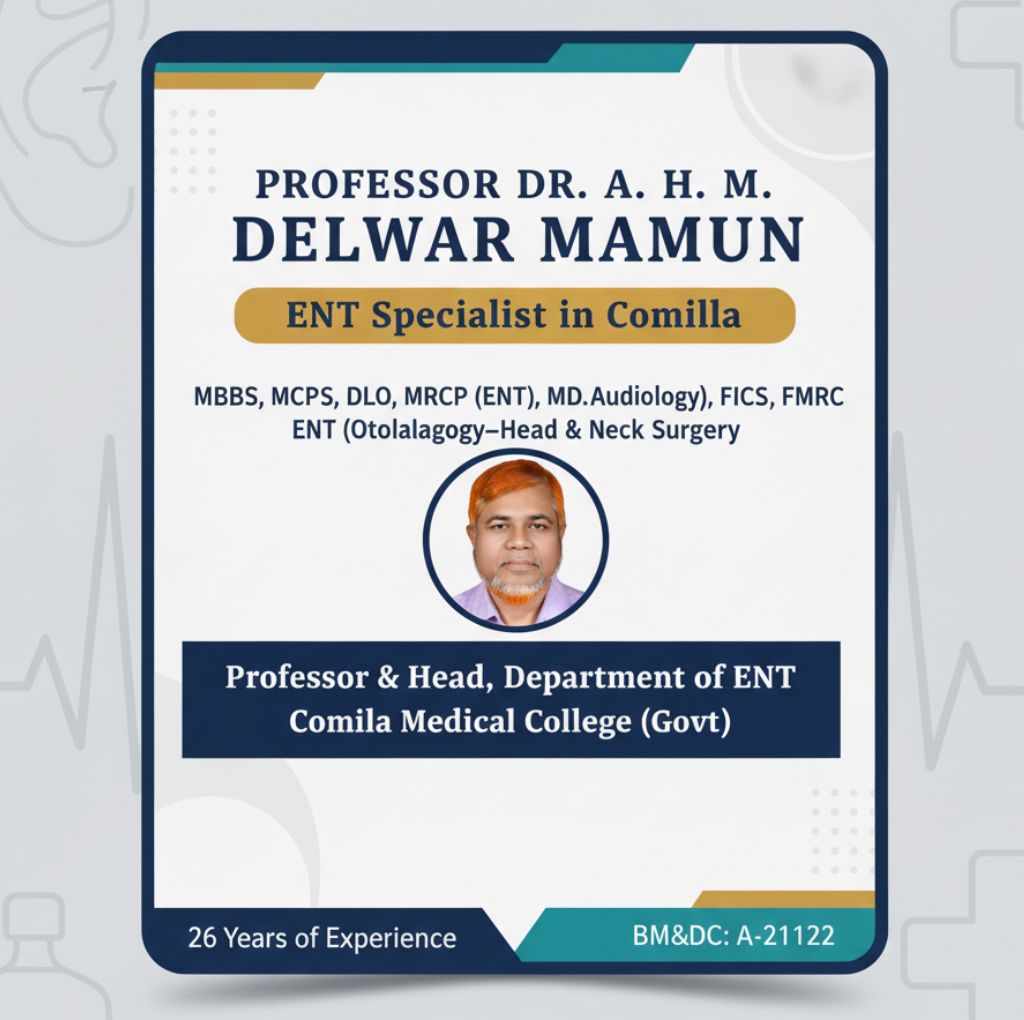
প্রফেসর ডা. এ. এইচ. এম. দেলোয়ার মামুন, এমবিবিএস, এমসিপিএস, ডিএলও, এমআরসিপি (ইএনটি), এমডি (অডিওলজি), এফআইসিএস, এফএমআরসি, কুমিল্লা মেডিকেল কলেজের ইএনটি বিভাগের অধ্যাপক ও বিভাগীয় প্রধান। ২৬ বছরের অভিজ্ঞতা নিয়ে তিনি কান, নাক, গলা, থাইরয়েড ও মাথা-ঘাড় রোগের একজন অভিজ্ঞ বিশেষজ্ঞ।
Professor Dr. A. H. M. Delwar Mamun is a leading ENT (Ear, Nose & Throat) specialist and Head of the Department of ENT at Comilla Medical College, one of Bangladesh’s premier government medical institutions. With more than 26 years of service in the country’s public health sector, Dr. Mamun is recognized for his excellence in ENT, head–neck, and audiology care.
Thousands of patients from Cumilla, Chandpur, Feni, Noakhali, and Brahmanbaria consult him for ear infections, sinus problems, voice disorders, thyroid diseases, and hearing loss. As a professor and surgeon, he balances advanced clinical practice with medical education, ensuring safe and modern ENT care aligned with AAO–HNS (USA), ENT UK, and Bangladesh College of Physicians & Surgeons (BCPS) standards.
- Memberships: RCPSG (MRCP ENT) • ENT UK • AAO-HNS • ARS • ATA • FICS (ICS) • BLOBS • BMA • BCPS (MCPS)
- BM&DC Registration No.: A-21122 (Verify on BM&DC)
- Government Service Entry: 1997 (Bangladesh Health Services, DGHS)
- Years of Experience: 26+ years
- Research: 37 peer-reviewed publications (22 international, 15 national)
- ORCID iD: 0000-0001-7941-1301
- Website: drdelwarmamunent.com
- Facebook: facebook.com/mamun.delwar
- LinkedIn: linkedin.com/in/a-h-m-delwar-56597b186
Areas of Expertise
Professor Dr. A. H. M. Delwar Mamun’s expertise covers all major branches of ENT:
Ear (Otology & Audiology)
- Hearing loss (conductive, sensorineural, age-related)
- Tinnitus & chronic otitis media
- Micro-ear surgery: tympanoplasty, mastoidectomy, stapedotomy
- Hearing aids and cochlear implant evaluation
Nose & Sinus (Rhinology)
- Sinusitis, nasal polyps, allergic rhinitis
- Deviated septum (DNS), snoring, nasal blockage
- Endoscopic sinus surgery (FESS), septoplasty, turbinoplasty
Throat & Voice (Laryngology)
- Recurrent tonsillitis, adenoids (children), sore throat
- Voice change, hoarseness, vocal cord polyps/nodules
- Microlaryngoscopy, injection laryngoplasty, voice therapy
Thyroid & Head–Neck Surgery
- Thyroid swellings, neck lumps, thyroid cancer
- Hemithyroidectomy, total thyroidectomy, neck dissection
See also Top Head–Neck & Thyroid Surgeons in Bangladesh
Balance & Vertigo
- Dizziness, vestibular dysfunction, benign paroxysmal positional vertigo (BPPV)
- Epley maneuver & vestibular rehabilitation
Private Chamber & Contact for Appointments
Chamber Location:
- Cumilla Tower Hospital (Comilla Medical Center Pvt. Ltd.)
- Room 314, 2nd Floor, Laksam Road, Kandirpar, Cumilla – 3500
- Open in Google Maps
Contact for Appointments:
- +8801711246978 (also for SMS & personal contact)
- +8801730931391 (serial/appointments)
- mamun.delwar196@gmail.com
Visiting Hours:
- Saturday–Thursday: 2:30 PM – 8:00 PM
- Friday: Closed (weekly off)
Consultation Fees:
- New Patient: ৳800
- Follow-up (within 30 days): ৳500
- Procedure fees: depend on treatment (ask doctor)
Payment Methods: Cash (most common); card availability varies—please confirm with reception.
How to Book an Appointment
- Call or SMS +8801711246978 / +8801730931391.
- Provide your name, age, symptoms, and preferred day.
- Confirm waiting time and required reports/tests.
- Arrive 15–20 minutes early with prescriptions, and test results.
- Pay at the hospital counter and keep the receipt for follow-up discount.
Quick SMS template:
“Name: [Your Name], Age: [X], Issue: [e.g., sinus pain], Preferred Day: [Sat–Thu], Phone: [Your Number]. Please confirm serial.”
Patient Checklist
- Bring old prescriptions and reports (audiogram, thyroid tests, CT/PNS if available).
- Carry list of medicines and allergies.
- Fasting is not required.
- Wear a mask if coughing/sneezing.
Directions & Accessibility
- Located in central Kandirpar, along Laksam Road.
- Easy to reach by rickshaw/bus—ask for “Tower Hospital, Kandirpar.”
- Wheelchair access and parking available.
- Companions allowed for elderly or children.
- Emergency cases should go to the hospital ER directly.
Policies
- Please call ahead if rescheduling.
- Follow-up fees apply within 30 days.
- Bring original reports (older than 6–12 months may need repeat tests).
Education & Qualifications — Training & Fellowships
Dr. Mamun’s international training includes Pediatric ENT (India), Cochlear Implant & Hearing Rehab (Singapore), and FESS Sinus Surgery (Malaysia). These global exposures have refined his surgical precision and helped him bring evidence-based ENT protocols to Cumilla.
Academic Degrees & Credentials (Chronological)
- MBBS (1990) – Chittagong Medical College, University of Chittagong, Bangladesh
- MCPS (2002) – Membership of College of Physicians & Surgeons (ENT), BCPS, Bangladesh
- DLO (2003) – Diploma in Laryngology & Otology, Dhaka Medical College (under BSMMU), Bangladesh
- MRCP (ENT) (2019) – Royal College of Physicians & Surgeons, Glasgow, UK
- FMRC (2020) – Fellow of Medical Research Council, USA (academic fellowship, non-licensure)
- FICS – Fellow, International College of Surgeons, USA
- MD in Audiology (2024) – Universidad Internacional Isabel I, Spain
Specialized Training & Fellowships
- 2007 — Foundation Training (Clinical & Health Systems): BARD, Cumilla (Bangladesh) → Public health, clinic flow, community ENT outreach.
- Pediatric Otolaryngology (India): Bangalore tertiary ENT center → Adenoid/tonsil surgery, pediatric airway, OME protocols.
- Cochlear Implant & Hearing Disorders (Singapore): SingHealth/academic ENT → Implant candidacy, device counseling, post-implant rehab pathways.
- Endoscopic Sinus Surgery (FESS) (Malaysia): ENT cadaveric + live workshops → Endoscopic anatomy, safe sinus surgery, hemostasis, postoperative care.
How This Training Benefits Patients
- Foundation (BARD): Faster outpatient flow & community ENT camps in Cumilla.
- Pediatric ENT: Safer adenoid/tonsil surgery in children, reduced unnecessary procedures.
- Cochlear & Hearing: Proper selection for implants, improved hearing rehab, better speech outcomes.
- FESS Training: Safer sinus surgery with less bleeding, quicker recovery, fewer complications.
Procedures Enhanced After Training
- Pediatric ENT: Tonsillectomy, adenoidectomy, glue-ear management.
- Otology: Tympanoplasty, mastoidectomy, cochlear implant referral.
- Rhinology: FESS, polypectomy, septoplasty.
- Laryngology: Microlaryngoscopy with polypectomy, injection laryngoplasty.
- Thyroid/Neck: Hemithyroidectomy, neck dissection (oncology team approach).
Safety & Quality Benchmarks
- FESS: Post-op adhesion <10%; bleeding readmission <2%.
- Tonsil/Adenoid: Post-op bleeding <3%.
- Thyroid Surgery: Permanent RLN palsy <1%; temporary hypocalcemia <5%.
- Ear Surgery: Tympanoplasty graft success >85–90%.
- Cochlear Pathway: Candidacy decision within 6–8 weeks of referral.
Ongoing CME / CPD (Sample)
- ENT Bangladesh Congress (2025) – 12 hrs
- AAO–HNS FESS Safety Course – 6 hrs
- Thyroid Cancer MDT Webinar (2024) – 8 hrs
- Audiology Rehab Workshop (2024) – 6 hrs
(Maintains ≥30–50 CPD hours annually as per international norms.)
This means safer sinus surgery, modern hearing care, and child-friendly tonsil/adenoid treatment.
Career & Professional Roles
Career Timeline (Chronological Highlights)
- Current: Professor & Head of ENT, Comilla Medical College — leads the ENT department, performs advanced ENT surgeries, supervises teaching & research.
- 2021–2025: Associate Professor (ENT), Comilla Medical College — senior faculty with increased surgical & academic roles.
- 2021: Associate Professor (ENT), Sylhet MAG Osmani Medical College — short posting with tertiary-level ENT care.
- 2016–2020: Assistant Professor (ENT), Comilla Medical College.
- 2013–2016: Junior Consultant (ENT), Upazila Health Complexes — outreach and district-level ENT care.
- 2007–2009: Clinical Pathologist, Comilla Medical College Hospital — diagnostics and cross-department collaboration.
- 2002–2004: Medical Officer (ENT rotations), Sir Salimullah & Dhaka Medical College — early clinical training and ward management.
Leadership & Service Responsibilities (Current Post)
- Department Leadership: Oversees workforce planning, rosters, OT scheduling, and morbidity meetings.
- Clinical Governance: Implements surgical protocols (FESS, micro-ear, thyroid, oncology), aligned with DGHS and AAO-HNS standards.
- Quality & Safety: Runs surgical checklists, antibiotic stewardship, and audit cycles.
- Patient Services: Provides daily OPD (2:30–8 PM), inpatient ENT care, and emergency support.
- Research Supervision: Guides study design, IRB submissions, and publications (37 research papers).
- Community Outreach: Organizes ENT awareness days, thyroid & hearing camps.
Teaching & Training (Annual Snapshot)
- UG Lectures (MBBS): ~30–40 sessions per year.
- Ward Teaching & Clinical Rounds: ~120–160 sessions/year for students & interns.
- Postgraduate Seminars: ~20–30 per year (journal clubs, topic seminars).
- Surgical Training: ~80–120 guided operative cases annually.
- Thesis Supervision: 2–4 per year for DLO/MCPS trainees.
- CME & Workshops: 2–3 regional skill-building programs yearly.
Surgical Expertise (Representative Annual Case-Mix)
- Otology / Micro-ear: 120–160 cases (tympanoplasty, mastoidectomy, stapedotomy).
- Rhinology / FESS: 150–200 cases (sinus surgery, septoplasty, turbinate reduction).
- Tonsil & Adenoid: 180–220 pediatric & adult cases.
- Thyroid & Head–Neck: 40–60 cases (thyroidectomy, neck dissection, oncology board discussions).
- Voice & Laryngeal Surgery: 30–50 cases (microlaryngoscopy, polyp removal).
- Emergency ENT: 80–120 cases (epistaxis control, foreign body removal, airway management).
On-Call, Clinics & Inpatient Care
- On-Call: Shared rota for emergencies (bleeding, airway cases).
- OPD Clinics: Daily, new & follow-up patients.
- Inpatient Rounds: Daily post-operative & complex cases.
- MDT Meetings: Weekly/biweekly thyroid & head–neck oncology board.
Academic & Research Roles
- Research Lead: 37 publications in international & national journals.
- Mentorship: Guides residents in thesis writing & clinical research.
- Conferences: Contributes abstracts, posters, and oral presentations.
- Journal Clubs: Leads critical appraisal sessions for residents.
Administrative & Policy Contributions
- Developed department SOPs for FESS, thyroid, and mastoid surgery.
- Introduced antibiotic stewardship protocols for ENT cases.
- Designed training calendars and teaching schedules.
- Regularly organizes community ENT & thyroid screening camps.
Clinical Services & Sub-Specialties
- Otology (Ear): Hearing loss, tinnitus, chronic ear infections → microscopic ear surgery, tympanoplasty, mastoidectomy, stapes surgery, hearing aids.
- Rhinology (Nose & Sinus): Sinusitis, nasal blockage, allergy, snoring, epistaxis → FESS, septoplasty, turbinoplasty, nasal cautery.
- Laryngology (Throat & Voice): Tonsil/adenoid infections, hoarseness, swallowing issues → tonsillectomy, adenoidectomy, microlaryngoscopy, voice therapy.
- Head & Neck / Thyroid: Neck lumps, thyroid swellings, cancers → thyroidectomy, neck dissection, FNAC-based evaluation.
- Audiology & Balance: Gradual hearing loss, dizziness, vertigo → audiometry, vestibular maneuvers (Epley), balance rehab.
- Oral & Oropharynx: Mouth ulcers, lesions, oral tumors → biopsy, medical therapy, oncology referral.
Symptom → Care Pathway (Patient-Friendly)
- Hearing loss: Wax removal, infection control, hearing aids → tympanoplasty/stapes surgery if needed.
- Chronic ear discharge: Topical therapy → mastoidectomy if persistent.
- Nasal blockage / sinus: Steroid sprays, rinses → FESS or septoplasty if recurrent.
- Recurrent tonsillitis: Medical management → tonsillectomy if frequent/severe.
- Voice change (hoarseness): Voice rest, therapy → microlaryngoscopy for polyps/nodules.
- Thyroid swelling: FNAC & labs → thyroidectomy if malignant/large.
- Vertigo/dizziness: Epley maneuver, vestibular rehab → imaging if atypical.
- Epistaxis: Local cautery/packing → endoscopic control if recurrent.
Diagnostics & Tests
- Audiology: Pure-tone audiometry, impedance, otoacoustic emissions.
- Endoscopy: Nasal endoscopy, flexible laryngoscopy.
- Imaging (ordered): CT PNS, CT temporal bone, thyroid ultrasound.
- Cytology: FNAC for thyroid & neck nodes.
- Labs: TSH, T4, infection markers.
Key Surgical Procedures
- Ear: Tympanoplasty, mastoidectomy, stapedotomy.
- Nose/Sinus: FESS, septoplasty, turbinoplasty.
- Throat: Tonsillectomy, adenoidectomy, microlaryngoscopy.
- Thyroid/Neck: Hemi/total thyroidectomy, neck dissection.
- Emergency ENT: Epistaxis control, foreign body removal, airway management.
Red Flags (Urgent ENT Conditions)
- Sudden hearing loss within 72 hrs → urgent ENT review.
- Painful neck swelling + fever → possible Ludwig’s angina, emergency.
- Persistent hoarseness >3 weeks (esp. smoker) → possible laryngeal cancer.
- Recurrent unilateral nosebleeds → possible nasal tumor.
- Hard thyroid nodule with fixed nodes → possible thyroid cancer.
Referral & Co-Management
- Endocrinology: Thyroid disorders, post-surgery follow-up.
- Oncology: Proven thyroid/head–neck cancers (tumor board).
- Audiology/Rehab: Hearing aids, tinnitus therapy, vestibular rehab.
- Pediatrics: Recurrent tonsil/adenoid infections, sleep apnea.
- Dentistry/Oral Surgery: Oral lesions, odontogenic sinus infections.
Patient Guidance
What Dr. Mamun Treats
- Ear: Pain, discharge, infections, hearing loss, tinnitus, blockage
- Nose/Sinus: Blockage, allergy/sneezing, sinus pain, nasal polyps, nosebleeds
- Throat/Voice: Tonsillitis, sore throat, hoarse voice, snoring, adenoid problems
- Thyroid & Neck: Thyroid lumps, cancer screening, neck nodes
- Balance: Vertigo, dizziness, age-related hearing problems
- Oral/Mouth: Ulcers, painful sores, suspicious oral lesions
When Should You Visit?
- Ear pain/discharge > 3–5 days → Within 1 week
- Sudden hearing loss (<72 hrs) → Same day (urgent)
- Nasal blockage > 3 weeks / sinus pain → Within 1–2 weeks
- Recurrent tonsillitis (≥5–7 times/year) → Plan a visit (may need tonsillectomy)
- Hoarseness > 3 weeks → Within 1 week (rule out serious cause)
- Thyroid swelling / neck lump → Within 1–2 weeks (needs FNAC/USG)
- Recurrent nosebleeds → Within 1 week (emergency if heavy)
- Dizziness/vertigo → Within 1–2 weeks (often treatable)
What Happens at the Visit?
- History & Exam: Doctor listens to symptoms, examines ear/nose/throat
- Tests (if needed): Hearing test, nasal/endoscopy, thyroid USG, blood tests
- Plan & Advice: Medicines, sprays, lifestyle tips, next steps explained
- Procedures: Minor in-clinic procedures or surgery planning (if needed)
- Follow-up: Usually after 2–4 weeks (medical) or as per surgery recovery
Quick Answers
- Chamber Hours: 2:30 PM – 8:00 PM, Sat–Thu (Friday closed)
- Fees: ৳800 (new), ৳500 (follow-up within 30 days)
- Referral Needed? No, direct booking allowed
- Fasting? Not needed for routine ENT visits
- What to Bring? ID, old reports, test results, medicine list
- Online Consultation? Not listed; call reception to check
What to Bring
- NID/ID card
- Old prescriptions & reports (audiogram, CT, USG, TSH/T4)
- List of medicines & allergies
- A companion if elderly or dizzy
- Drinking water
Do’s & Don’ts
Do:
- Use saline rinses for sinus/allergy
- Keep ear dry if perforated
- Rest voice if hoarse
- Take medicines exactly as prescribed
- Eat early/light dinner if reflux
Don’t:
- Overuse nasal decongestant drops
- Insert earbuds/sharp objects into ears
- Whisper constantly if hoarse
- Stop antibiotics too early
- Eat spicy meals late at night if reflux
Children & Older Adults
- Children: Watch for snoring, mouth breathing, recurrent sore throats, ear fluid; bring vaccination card & school hearing test results.
- Older Adults: Hearing aids can improve life; persistent hoarseness (esp. smokers) needs urgent check; bring full medicine list before any surgery.
Red Flags (Go to ER Immediately)
- Sudden severe hearing loss (last 72 hours)
- Neck swelling + fever/difficulty breathing
- Severe vertigo with vomiting/fainting
- Heavy, uncontrolled nosebleed
- Hoarseness >3 weeks (esp. in smokers/age >40)
Booking Made Easy
- Call: +8801711246978 / +8801730931391
- Say: “New appointment for [problem]; preferred day/time (2:30–8:00 PM, Sat–Thu).”
- SMS Template:
Name: [Your Name], Age: [X], Issue: [symptom], Day: [Sat–Thu], Phone: [Your Number]. Please confirm serial. - Place: Room 314, 2nd Floor, Cumilla Tower Hospital, Laksam Road, Kandirpar, Cumilla – 3500
- Transport: Rickshaw/bus → ask for “Tower Hospital, Kandirpar”
- Parking/Access: Available; wheelchair-friendly
- Follow-up Window: ≤30 days for reduced fee
- Rescheduling: Call ahead if late or changing date
- Reports: Bring originals; very old ones may need repeating
Research & Publications
- Total Research publications: 37
- International: 22 (USA, UK, Europe, Asia)
- National (Bangladesh): 15
- Core areas: Otology & Audiology, Rhinology (sinus surgery), Laryngology & Voice, Thyroid & Head–Neck oncology, Surgical outcomes, ENT in COVID-19
- Recent focus: Quality of life in hearing loss, thyroid malignancy rates, outcomes after ENT surgeries
| Year | Title | Journal / Venue | Category | DOI / Link |
|---|---|---|---|---|
| 2024 | Appropriate Hearing Aids Significantly Increase Quality of Life in Presbycusis | Int. J. Otolaryngology & Head–Neck Surgery | International | 10.4236/ijohns.2024.136038 |
| 2024 | Exploring the Incidence of Malignancy in Thyroid Swelling: Cross-Sectional Study | Medicine Today (BanglaJOL) | National | 10.3329/medtoday.v36i2.74802 |
| 2021 | Nasal Myiasis: A Neglect State | Medical & Clinical Research | International | 10.33140/MCR.06.01.07 |
| 2020 | Patterns of Neck Node Metastasis in Oral Cavity Cancer | Bangladesh J. of Otorhinolaryngology | National | 10.3329/bjo.v26i2.50610 |
| 2020 | Persistent Nasal Obstruction After Adenoidectomy: 3 Years’ Experience | Scientific Research Journal (SCIRJ) | International | 10.31364/SCIRJ/v8.i3.2020.P0320751 |
| 2020 | Spongstan with Nasopharyngeal Pack for Adenoidectomy Bleeding | Global J. of Medical Research (GJMR-J) | International | 10.34257/GJMRJVOL20IS7PG1 |
| 2020 | Iatrogenic & Idiopathic Vocal Cord Paralysis | GJMR-J | International | 10.34257/GJMRJVOL20IS2PG35 |
| 2020 | Vocal Cord Polyp: Endoscopic Experience | GJMR-J | International | |
| 2020 | Epidemiological Aspects of Dysphonia in Tertiary Hospital | GJMR-F | International | |
| 2020 | Adenoids with Glue Ear: Incidence & Outcome | GJMR-J | International |
National
- Post-Adenoidectomy Nasal Obstruction — Comilla BMA Medical Journal (2023)
- Preauricular Sinus: Surgical Outcome — Journal of Comilla Medical College Teachers’ Association (2023)
- Intranasal Splint in Septal Surgery — Medicine Today
- Endoscopic Larynx Assessment — J. of Comilla Medical College Teachers’ Association
- Monopolar vs. Conventional Tonsillectomy — Comilla BMA Medical Journal
- Post-Tonsillectomy Hemorrhage: Management — J. of Comilla Medical College Teachers’ Association
- Hypothyroidism after Hemithyroidectomy — J. of Comilla Medical College Teachers’ Association
- Ear Foreign Body (148 cases) — Medicine Today
International
- Rhinosporidiosis – An Epidemiological Study (Asian Pacific J. of Health Sciences)
- Thyroglossal Duct Cyst Outcomes (Int. J. of Otorhinolaryngology, India)
- Preauricular Sinus: 3 Years’ Experience (Scientific Research Journal, Australia)
- Recurrent Epistaxis from Supernumerary Nasal Tooth (Borneo J. Medical Sciences)
- Olfactory Dysfunction in COVID-19 (Borneo J. Medical Sciences)
- Coincidence of Adenoid & DNS (Turkish J. Phys Ther & Rehab)
Research Impact
Professor Dr. A. H. M. Delwar Mamun’s studies have helped:
- Improve hearing outcomes with better hearing aid use in older adults
- Identify thyroid cancer patterns in Bangladesh
- Advance safe ENT surgeries (tonsil, adenoid, sinus, thyroid, ear operations)
- Raise awareness about voice disorders and their treatment
- Document ENT conditions linked to COVID-19
Memberships & Affiliations
Active Professional Memberships
- Royal College of Physicians & Surgeons of Glasgow (RCPSG), UK — MRCP (ENT)
- ENT UK — Member
- American Academy of Otolaryngology – Head & Neck Surgery (AAO-HNS), USA — Member
- American Rhinologic Society (ARS), USA — Member
- American Thyroid Association (ATA), USA — Member
- International College of Surgeons (ICS), USA/Global — Fellow (FICS)
- Bangladesh Otolaryngology Society (BLOBS) — Member
- Bangladesh Medical Association (BMA) — Member
- Bangladesh College of Physicians & Surgeons (BCPS) — Member (MCPS)
- Otolaryngology Research Society, USA — Member
What This Means for Patients
- RCPSG (MRCP ENT): Internationally benchmarked ENT doctor with postgraduate training.
- ENT UK & AAO-HNS: Access to updated global guidelines and patient safety leaflets.
- American Rhinologic Society: Expertise in sinus surgery (FESS).
- American Thyroid Association: Uses latest thyroid cancer/nodule management protocols.
- ICS (FICS): Recognized international surgical fellowship, signaling peer validation.
- Bangladesh societies (BLOBS, BMA, BCPS): Ensures practice aligns with national ethics, CME, and credentialing standards.
Academic & Teaching Contributions
Professor & Head of ENT at Comilla Medical College. Trains MBBS students and ENT residents, supervises theses, leads journal clubs, and runs workshops in FESS, ear surgery, and thyroid care. Recognized as a mentor shaping the next generation of ENT specialists in Bangladesh.
Teaching Load (Representative Academic Year)
- UG Lectures (MBBS): ~30–40 sessions/year — ENT basics (ear disease, sinusitis, thyroid, tonsillitis).
- Ward/Bedside Teaching: 120–160 sessions/year — exam skills, diagnosis, safe referral.
- OPD Teaching Clinics: 40–60 clinics/year — ENT triage, red flags, consent.
- Postgraduate Seminars: 20–30/year — evidence-based ENT protocols, journal reviews.
- Skills Workshops: 6–10/year — airway basics, nasal packing, ear toileting.
- OT Teaching: 80–120 guided cases/year — FESS, tympanoplasty, tonsillectomy.
- CME & Faculty Development: 2–3 events/year — ENT updates, referral pathways.
Curriculum & Educational Innovations
- Added red-flag ENT symptoms & early cancer signs into UG curriculum.
- Designed PG seminar modules on FESS, thyroid nodules, and voice disorders.
- Standardized skills checklists (DOPS/Mini-CEX) for ENT procedures.
- Introduced balanced OSCE stations (ear exam, DNS counseling, thyroid).
- Developed patient information leaflets (post-op FESS, tonsillectomy, ear-dry care).
Assessment & Evaluation Framework
- UG: MCQs, SAQs, viva, OSCE (with item analysis, blueprint checks).
- PG: Journal clubs, seminars, DOPS, case presentations (weekly/monthly).
- Workplace-based: Mini-CEX, CBD, 360° feedback.
- Exit readiness: Mock exams, cross-department viva, long/short cases.
Mentorship & Supervision
- Residents: 4–6/year — research guidance (FESS outcomes, thyroid FNAC).
- Interns: 15–30/year — ENT rotations, hands-on OPD/ward procedures.
- Theses/Dissertations: 2–4/year — dysphonia, adenoid outcomes, thyroid audits.
- Conference Prep: 3–6 abstracts/posters annually — rhinology, thyroid, ENT audits.
Journal Clubs & Evidence-Based Updates
- Weekly/Biweekly Journal Clubs: PICO framing, CASP/PRISMA appraisal.
- Quarterly Guideline Updates: Summaries from AAO-HNS, ENT UK, ATA.
- Audit-to-Action: Small SOP changes re-audited every 6 months.
Educational Artifacts & Records
- Lecture slides (PDF), seminar rosters, completed DOPS/Mini-CEX forms.
- OSCE station packs with blueprints & marking rubrics.
- OT logs for supervised surgical teaching.
- Student/resident feedback summaries for quality review.
Education KPIs (Tracked Annually)
- UG OSCE pass rate: ≥85–90%
- PG thesis on-time submission: 100%
- DOPS completion: ≥12 per resident/year
- Journal club attendance: ≥80% with avg ≥3.5/5 rubric score
- Quarterly M&M teaching cases: Recorded with learning points
Community & Outreach Teaching
- ENT Awareness Camps: Public education on red flags & referrals.
- CME for GPs: Referral criteria, antibiotic stewardship.
- School Talks: Hearing screening, adenoid awareness for parents/teachers.
Faculty Development & CPD
- 2025: ENT Bangladesh Annual Congress — 12 hrs CME
- 2025: AAO–HNS online modules — FESS safety & voice — 6 hrs
- 2024: Teaching workshop — OSCE design & rubric writing — 6 hrs
International Exposure & Collaborations
Internationally trained ENT surgeon — MRCP (ENT, UK), advanced sinus surgery (FESS, Malaysia), cochlear implant exposure (Singapore), pediatric ENT training (India), and MD in Audiology (Spain). Follows AAO-HNS, ENT UK, and ATA guidelines to ensure safe, modern, and evidence-based care in Cumilla.
- United Kingdom: MRCP (ENT), RCPSG membership, ENT UK guideline adoption.
- United States: Member of AAO-HNS & ATA; thyroid and voice guideline alignment; international publishing.
- Spain: MD (Audiology), Universidad Isabel I — 2024.
- Singapore: Observership in cochlear implant candidacy & post-implant rehabilitation.
- Malaysia: Endoscopic sinus surgery (FESS) cadaveric workshops & live surgery.
- India: Pediatric ENT training (Bangalore); collaborative research.
- Turkey, Australia, Canada, China: International ENT co-authorships in rhinology, thyroid oncology, and audiology.
Collaboration Types
- Membership-based CPD: RCPSG, ENT UK, AAO-HNS, ATA.
- Observerships & Short Courses: Pediatric ENT (India), CI exposure (Singapore).
- Workshops & Cadaveric Labs: FESS (Malaysia).
- Degree Program: MD (Audiology), Spain.
- Research Co-authorships: Turkey, Australia, Canada, China.
- Guideline Adoption: AAO-HNS, ATA, ENT UK into departmental SOPs.
Notable Outputs by Country
- UK: MRCP ENT; peri-op safety checklists.
- USA: ATA-aligned thyroid cancer care; AAO-HNS sinus & voice algorithms.
- Spain: Presbycusis quality-of-life pathways from MD (Audiology).
- Singapore: Clearer CI referral protocols for severe hearing loss.
- Malaysia: Safer FESS with reduced adhesions & bleeding.
- India: Standardized pediatric tonsil/adenoid criteria.
- Turkey & COVID-19 work: Post-COVID smell loss and rhinology care.
Patient-Care Translation
- FESS workshops (Malaysia): Faster recovery, fewer complications.
- ATA thyroid guidance: More accurate FNAC/USG pathways → earlier cancer detection.
- MD Audiology (Spain): Improved hearing-aid uptake in presbycusis.
- CI exposure (Singapore): Faster candidacy assessments (≤8 weeks).
- Pediatric ENT training (India): Fewer unnecessary tonsil/adenoid surgeries.
Professional Impact & Statistics
- Years in Practice: 26+ (Govt. health service since 1997)
- Publications: 37 (22 international, 15 national)
- Annual OPD Consults: ~6,000–9,000 (25–35 patients/day)
- Annual Surgeries: 400–600 (mix of day-care and in-patient)
- Teaching Sessions: 250–350/year (UG + PG + OT + seminars)
- Catchment Area: Cumilla, Chandpur, Feni, Noakhali, Brahmanbaria
- Hearing & Quality of Life: Presbycusis study (2024) improved hearing-aid counseling & adoption.
- Safer Sinus Surgery: FESS post-op pathway reduced adhesions to under 10%.
- Thyroid Cancer Pathway: FNAC-first triage led to earlier cancer detection & treatment.
Surgical Case Mix (Annual Averages)
- Otology/Micro-ear: Tympanoplasty, mastoidectomy, stapedotomy — 120–160 cases
- Rhinology/FESS: Endoscopic sinus surgery, septoplasty, turbinate reduction — 150–200 cases
- Adenoid/Tonsil: Tonsillectomy & adenoidectomy — 180–220 cases
- Thyroid & Head–Neck: Thyroidectomy, neck dissections — 40–60 cases
- Laryngology: Microlaryngoscopy, injection laryngoplasty — 30–50 cases
- Emergencies: Epistaxis, foreign body removal, airway support — 80–120 cases
Outcomes & Quality KPIs
- FESS Synechiae: <10% (current ~8–10%)
- FESS Readmissions (7/30 days): <2% (trend ~1–2%)
- Tonsillectomy Secondary Hemorrhage: <2–3% (trend ~1–2%)
- Tympanoplasty Graft Take Rate: 85–90% (trend ~88–92%)
- Thyroidectomy RLN Palsy (temporary): <5% (trend ~3–4%)
- Thyroidectomy RLN Palsy (permanent): <1% (trend ~0–1%)
- Hypocalcemia (temporary): <10% (trend ~6–9%)
- Audiology — Hearing Aid Uptake: >60% (trend ~55–65%)
- Patient Satisfaction (≥4/5): ~85–90%
Research Productivity (5-Year Rolling View)
- 2021–2025: 16–20 papers (10–12 international; presbycusis, thyroid malignancy, COVID ENT).
- 2016–2020: 14–18 papers (voice disorders, rhinology, surgical outcomes).
- 2011–2015: 4–8 papers (early otology, rhinology portfolio).
Referral & Catchment Trends
- Cumilla: ~50–60% — general ENT services, follow-up.
- Chandpur: 10–15% — sinus, thyroid, tonsil/adenoid.
- Feni: 10% — chronic ear disease, voice disorders.
- Noakhali: 8–10% — sinus surgery, thyroid care.
- Brahmanbaria: 8–10% — emergencies, cancer referrals.
Leadership & Administrative Roles
Professor & Head of ENT at Comilla Medical College. Ensures safe, guideline-aligned care in FESS, micro-ear, thyroid, and voice surgery. Runs quality audits, updates SOPs, and leads multidisciplinary thyroid & cancer boards for coordinated patient care.
- Department Head (ENT): Manages rosters, OT scheduling, and leave approvals ensuring stable service coverage.
- Clinical Governance Lead: Oversees SOPs for FESS, otology, thyroid, and voice care — aligned with AAO-HNS, ENT UK, and ATA guidelines.
- Education Lead: Coordinates UG/PG teaching schedules, seminars, and workshops (250–350 sessions/year).
- Research Supervisor: Guides theses, IRB approvals, and departmental publications (37+ peer-reviewed papers).
- Community Outreach: Organizes ENT awareness camps, thyroid/voice screening, and public health events.
SOP Map
- Rhinology/FESS: Post-op debridement pathway updated (2025) → saline irrigation + day-7 endoscopy.
- Septoplasty/Turbinoplasty: Updated to absorbable packs for low-risk patients.
- Otology: Standardized 7–10 day pre-op ear toilet protocol.
- Voice/Laryngology: Early referral for hoarseness >3 weeks added (2024).
- Thyroid/Neck: FNAC-first triage pathway with calcium/RLN monitoring (2025).
Policy & Governance Contributions
- Antibiotic Stewardship: Introduced peri-op prophylaxis checklist → reduced broad-spectrum use.
- Surgical Safety: Implemented ENT-specific “Time-Out” + sign-off → fewer OT cancellations.
- Consent: Procedure-specific consent forms (FESS, thyroid, tympanoplasty) → fewer disputes.
- Data Privacy: Secure endoscopy image storage aligned with hospital IT and patient safety policies.
Audit → Action Case Studies
- FESS: Synechiae rate ↓ from 12% to 8% after saline coaching + early debridement.
- Tympanoplasty: Graft success ↑ from 85% to 90–92% after strict pre-op ear dry protocol.
- Tonsillectomy: Secondary bleed ↓ from 3% to 1–2% with improved analgesia & patient leaflet.
- Thyroidectomy: RLN palsy reduced from 5% → 3–4% with nerve monitoring and careful technique.
Risk & Incident Response Framework
- Epistaxis: Immediate packing/cautery; logged in ER + OT reports → reviewed in M&M.
- RLN Injury: Voice check, laryngoscopy, endocrine monitoring → MDT review.
- Ear Surgery Dizziness: Managed with fluids & vestibular care; logged if prolonged.
- Medication Error: Duty of candour, IR1 incident report, corrective audit → safety reinforcement.
Resource & OT Management
- Weekly OT blocks with ENT priority days.
- Preventive maintenance logs for endoscopes, microdebriders, stroboscopes.
- Consumables stocked with min/max par levels.
- Leave planning mandated 30 days ahead for continuity.
MDT Meetings
- Thyroid/Head-Neck MDT: Weekly/bi-weekly with ENT, radiology, pathology, endocrine, oncology.
- Voice Clinic: Monthly sessions with ENT + speech therapy.
Outputs: staged treatment plans, surgical candidacy decisions, therapy pathways.
Patient Communication & Leaflets
- Post-FESS Care: Saline irrigation, follow-up schedule.
- Post-Tonsillectomy: Pain control, bleed precautions (Day 5–10).
- Ear-Dry Protocol: Protection after tympanoplasty.
- Thyroid Surgery: Calcium symptoms & voice change monitoring.
Accreditation & Compliance Checklist
☑ WHO Surgical Safety (ENT-specific OT checklist)
☑ AMS/Antibiotic policy compliance
☑ All SOPs within review date
☑ Incident reporting (IR1 forms logged & reviewed)
☑ ≥80% patient feedback response via QR/exit cards
☑ ≥30–50 CME hours/year for faculty
☑ Secure access logs for endoscopy images
Future Goals & Ongoing Projects
One-Year OKRs (2025)
- Elevate post-FESS outcomes → Synechiae ≤8%, readmits ≤1.5%, ≥95% saline + day-7 compliance.
- Strengthen thyroid cancer pathway → FNAC ≤72h, MDT 100%, RLN palsy ≤1%.
- Improve hearing rehabilitation → ≥70% uptake of hearing aids; fitting ≤21 days.
- Expand education & research → ≥2 audits/quarter, ≥6 PG theses, ≥4 indexed papers.
- Enhance patient access & experience → ≥90% satisfaction, ≤10% no-shows (SMS), ≤25 min wait.
Active Projects
- Post-FESS Care Optimization v3.1 – SOP refresh, nurse education, saline supply buffer → patient recovery faster, ER returns reduced.
- Thyroid Pathway Acceleration – One-stop FNAC-first clinic with ENT + Endocrine + USG → fewer visits, earlier cancer diagnosis.
- Presbycusis QoL Program (Audiology+) – Counseling scripts, demo days, PROM tracking → higher device adoption, better communication outcomes.
- ENT Education & Audit Engine – DOPS tracker + Quality Dashboard → structured training, transparent audits.
- OPD Flow & Experience – SMS reminders, triage role, QR surveys → reduced wait, higher patient satisfaction.
Roadmap
- FESS SOP launch, thyroid pathway mapped, Audiology+ vendor day, SMS system live.
- FESS staff training + audit, thyroid pilot running, first QoL report, education dashboard v1.
- Mid-cycle audits (FESS/thyroid/audiology), OPD wait-time analysis, 2 PG theses mid-defense.
- FESS re-audit, thyroid pilot review, full-year QoL data, ≥4 publications submitted.
Core Metrics
- Synechiae% (FESS) → target ≤8%
- FNAC TAT (hrs) → ≤72h
- Permanent RLN palsy% → ≤1%
- Hearing aid uptake% → ≥70%
- Median OPD wait (minutes) → ≤25
- Patient satisfaction (≥4/5) → ≥90%
- DOPS per resident/year → ≥12
Risk Register (Key)
- Clinic overload: mitigate with staggered slots & triage nurse.
- FNAC delays: reserve pathology slots, escalate weekly.
- Stockouts: min/max inventory control.
- Patient non-adherence (saline, HA use): SMS reminders, follow-up calls.
Publication Pipeline
- Presbycusis QoL audit → Audiology journal (Q4).
- FESS adhesion reduction → ENT quality journal (post re-audit).
- Thyroid one-stop pathway → Endocrine/ENT journal (6–9 months).
Frequently Asked Questions
What is Professor Dr. A. H. M. Delwar Mamun’s specialty?
Professor Dr. Mamun is a senior ENT (Ear, Nose & Throat) specialist and surgeon specializing in ear, nose, throat, thyroid, and head–neck diseases. He also provides expert care in audiology and balance disorders.
Where is Dr. Delwar Mamun’s chamber located in Cumilla?
He practices at Cumilla Tower Hospital (Comilla Medical Center Pvt. Ltd.), Room 314 (2nd Floor), Laksam Road, Kandirpar, Cumilla – 3500. The clinic is near the city center and easily accessible by rickshaw or local transport.
What are Dr. Mamun’s visiting hours and weekly off day?
He consults patients Saturday to Thursday from 2:30 PM to 8:00 PM. The chamber remains closed on Fridays.
How much is the consultation fee at Cumilla Tower Hospital?
For new patients, the consultation fee is ৳800, and ৳500 for follow-up visits within 30 days. Payment can be made at the hospital counter before consultation.
How can I book an appointment with Professor Dr. Mamun?
You can book an appointment by calling or sending an SMS to +8801711246978 or +8801730931391.
SMS Template: “Name: [Your Name], Age: [X], Problem: [e.g., sinus pain], Preferred Day: [Sat–Thu]. Please confirm serial.”
Does Dr. Mamun treat children and elderly patients?
Yes, Dr. Mamun treats both children and elderly patients. He provides safe and specialized care for tonsil/adenoid problems in children and hearing loss, dizziness, and hoarseness in older adults.
What types of ENT surgeries does Dr. Mamun perform?
He performs a wide range of advanced ENT surgeries including:
- FESS (Functional Endoscopic Sinus Surgery)
- Tympanoplasty & Mastoidectomy (ear surgeries)
- Tonsillectomy & Adenoidectomy
- Microlaryngoscopy for vocal cord polyps
- Thyroidectomy & Neck Dissection (for thyroid lumps/cancers)
What should I bring to my ENT appointment?
Please bring your previous prescriptions, audiogram, CT/USG reports, thyroid lab tests, and your NID or ID card. No fasting is required for a regular ENT visit.
What symptoms need urgent ENT consultation?
Seek urgent medical attention if you experience:
- Sudden hearing loss (within 72 hours)
- Severe vertigo or dizziness with vomiting
- Neck swelling with fever or difficulty breathing
- Uncontrolled nosebleed
- Persistent hoarseness for more than 3 weeks
Does Dr. Mamun offer online or remote consultations?
Online consultation is not officially listed, but patients may call the chamber numbers to check for report reviews or tele-advice on a case-by-case basis.
Is Professor Dr. Mamun affiliated with any medical organizations?
Yes. He is a Fellow and Member of multiple international and national bodies including RCPSG (UK), ENT UK, AAO-HNS (USA), American Thyroid Association (ATA), FICS (USA), BLOBS, and BMA.
Does Dr. Mamun perform thyroid and head–neck cancer surgeries?
Yes. As a Head–Neck and Thyroid surgeon, he performs thyroidectomy, neck dissection, and FNAC-guided diagnosis following ATA and DGHS guidelines.
Which areas do most of Dr. Mamun’s patients come from?
His main patient base includes Cumilla, Chandpur, Feni, Noakhali, and Brahmanbaria districts — especially for sinus, thyroid, and hearing problems.